
Postoperative outcomes of intracranial stenting are worse when the procedure is performed in clinical practice rather than in the context of a trial, according to a large study appearing online this month in the journal Stroke. Researchers led by the University of Minnesota’s Dr. Farhan Siddiq halted their SAMMPRIS (Stenting and Aggressive Medical Management for […]
 Postoperative outcomes of intracranial stenting are worse when the procedure is performed in clinical practice rather than in the context of a trial, according to a large study appearing online this month in the journal Stroke.
Postoperative outcomes of intracranial stenting are worse when the procedure is performed in clinical practice rather than in the context of a trial, according to a large study appearing online this month in the journal Stroke.
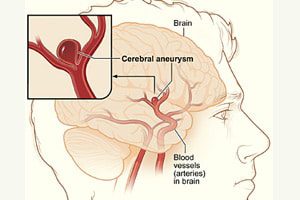
Researchers led by the University of Minnesota’s Dr. Farhan Siddiq halted their SAMMPRIS (Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis) trial early due to a higher 30-day rate of stroke and death with stenting compared to medical therapy, TCTMD reports.
Dr. Siddiq and colleagues examined records for 3,447 ischemic stroke patients from the National Inpatient Sample (NIS) who were treated with intracranial stenting from 2008 to 2010 either as part of (223) or outside (3,224) a clinical trial. The clinical trial patients were older (68 vs. 65 years), but sex and other baseline characteristics were similar in the two groups.
Medical therapy consisted of dual antiplatelet therapy and intensive management of primary and secondary risk factors. Many of the stent patients received either the Gateway PTA Balloon Catheter or the self-expanding Wingspan stent (both manufactured by Stryker Neurovascular of Kalamazoo, MI).
“Intracranial stent placement procedures outside a clinical trial have higher rates of postoperative stroke, cardiac complication, and mortality,” Dr. Siddiq and colleagues conclude, according to TCTMD. The “cherry-picking phenomenon” may be a factor, they say: patients treated within clinical trials have more favorable characteristics than those treated as a part of routine practice.
Stroke or death within 30 days occurred more than twice as often among stented patients than among those receiving medical therapy alone. The rate of any stroke was also higher in the stented group. In addition, there were five stroke-related deaths in the stented group compared with one non-stroke-related death in the medical management group.
The researchers say the discrepancy is not attributable to differences in the quality of the operators, since all were experienced and they had been involved in the earlier studies, according to TCTMD. But, the researchers explain, patients in the current trial had more severe stenoses and recent symptoms, and the trial’s rigorous neurological assessment may have detected more mild strokes.
In commenting on an earlier SAMMPRIS trial, Dr. Christopher J. White, of the John Ochsner Heart and Vascular Institute in New Orleans suggested that the trial results indicate the self-expanding Wingspan stent may not be the best device for intracranial intervention.


