
The issue of stenting overuse has become the focus of whistleblower lawsuits, federal lawsuits, and Department of Justice investigations. As we’ve written, the issue of cardiac stenting has highlighted potential overuse of the devices that may lead to cardiac complications. Cardiac stenting involves propping open a narrowed coronary artery with a small, metal mesh tube. […]
 The issue of stenting overuse has become the focus of whistleblower lawsuits, federal lawsuits, and Department of Justice investigations.
The issue of stenting overuse has become the focus of whistleblower lawsuits, federal lawsuits, and Department of Justice investigations.
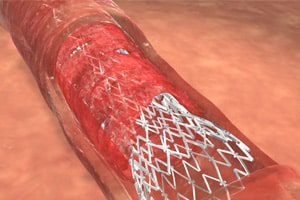
As we’ve written, the issue of cardiac stenting has highlighted potential overuse of the devices that may lead to cardiac complications. Cardiac stenting involves propping open a narrowed coronary artery with a small, metal mesh tube. During emergency surgery, for instance, when a patient is suffering a heart attack, a stent can save a life. Studies have long revealed, however, that stents are being implanted in patients who do not realize any significant benefit from stent implantation. About 700,000 stent procedures are conducted nationwide each year.
In just one stenting case on which Bloomberg.com reported, surgeon Najam Azmat allegedly tore a patient’s aorta, according to documents filed with a U.S. Justice Department civil complaint. Another surgeon was called in to complete the procedure at the request of the nursing team and that surgeon warned administrators at Satilla Regional Medical Center in Waycross, Georgia about Azmat. One nurse’s notes indicated that the hospital received seven similar warnings; Azmat continued working there and another patient died.
In that case, Azmat, has been accused of puncturing the wall of a patient’s right kidney during a stent procedure. The patient died 17 days later over heavy blood loss complications, according to the federal complaint, Bloomberg.com reported. The Justice Department’s expert report indicated that the procedure “was not medically indicated” and, according to Harold Kent, an expert witness for the plaintiff’s family, “People who should have and could have saved” the patient’s “life were too interested in having Dr. Azmat continue to do procedures and make money for the hospital to do the right thing.” Although the hospital denied wrongdoing, it did agree to pay $840,000 to resolve the Justice Department’s complaint that the facility submitted claims for cath-lab services, some not needed, that Azmat was neither qualified nor appropriately credentialed to perform, according to Bloomberg.com.
Based on numerous interviews, more than 1,000 pages of medical records, internal documents, and witness statements made public in 2012, the situation with Azmat and the Satilla Regional Medical Center is just one example of how far a facility went to maintain its catheterization clinic—also popularly known as a “cath lab.”
In other cases, Bloomberg.com reported on, hospitals paid millions of dollars in kickbacks in which ghost jobs were used and padded fees, debt forgiveness, and discounted office space were offered in efforts to ensure physicians kept conducting stent procedures, according to allegations in five federal cases and three private whistle blower lawsuits.
David Brown, a cardiologist at Stony Brook University School of Medicine in New York pointed out that, while some seven million heart patients have been implanted with catheters in the past 10 years, about one-third of those procedures were unnecessary. And, according to Bloomberg.com, 11 hospitals have agreed to settlements with the Justice Department to resolve civil allegations of unnecessary stenting and related issues. Many of the federal cases were filed by whistleblowers and, in information made recently public, documents show that hospitals benefited financially, sometimes ignoring or urging allegedly inappropriate use of stents.
The Department of Justice has been conducting investigations into interventional cardiology and stenting since 2006; no less than 11 hospitals have settled federal allegations they billed public health programs for unnecessary stents and related issues, according to Bloomberg.com previously. Investigations are ongoing in five other states.


